Parasites are usually macroscopic organisms of various genera that infect man, animals and plants, However, our interest in this chapter is on human parasites.
The process of examination of clinical specimens for parasites begins with parasite specimen collection. Again, two types of specimens are generally examined. These are fresh specimens and preserved specimens.
FRESH SPECIMEN COLLECTION
Clinical specimens for parasitological examination should be collected as soon as any abnormality is reported. This is to avoid any condition that would alter or modify the parasites following medication. For example stool specimens containing Barium are very difficult to examine as intestinal protozoa may not be detected till one week or more after the use of the barium compound. Other medication like mineral oil, bismuth, antibiotics and antimalarials cause similar situation.
Feacal specimens should be collected in clean, dry, wide mouthed containers with tight-fitting lid. This is to avoid spillage and preserve moisture in the specimen. Contamination with stream, pond or rain water containing free-living organism or urine which destroys motile organisms should be avoided.
Usually stool specimens are better examined fresh especially if trophozoites and flagellates are involved. Watery stools are better examined within 30mins -1h of collection (passage), soft specimens, 1h – 1 ½ h while formed specimens can take 2-3h.
Fresh specimen ensures easy identification of parasites as all features are still recognizable, since preservation even over night in refrigerators has adverse effect on trophic amoebae. Fresh specimen must be handled with care as they are potential sources of infection of laboratory staff.
PRESERVED SPECIMENS
Following pressure of work, late arrival of specimen, location of patient or any other reason, specimens may not be examined fresh hence preservation is necessary. There are many preservatives available but most are both preservative and at the same time fixatives. The best are those which can preserve protozoan/amoebae morphology and _ arrest further development of helminthic egg/ larvae.
Common preservatives used include formalin, polyvinyl alcohol (PVA), formalin, picric acid, shaudinn’s solution, formalin – alcohol – acetic acid (FAA) and Methiolate (thimerosal) – Iodine formation (MIF). Each of them has its own advantages and disadvantages but adequate mixing is important in which ever one chosen.
Three often used preservatives are:
a. PVA:
is a combination of a fixative and waterSoluble resin. It is best for liquid and semi-formed Specimens. It is good in cysts and trophozoite preservation and also enables permanent staining.
Add the PVA and cover the beaker or flask containers. Leave standing overnight and then slowly heat to 75°C and swirl. A slightly homog n us milky solution is obtained after 30 seconds to min. It is stabl f r6 months to 1 year.
FORMALIN
Formalin is 1 a eous or saline solution of formaldehyde. Cysts of prot 7 an helminth eggs and larvae are well preserved for long periods but not trophozoites. It is best to use warm or fairly hot formalin on fresh stool to arrest further development of helminth eggs to infective stages.
The specimen may be strained through a guaze before application of the formation in a cone-shaped container and allowed to stand for one-two hours before preservation to concentrate the parasites. Formalin preserved specimens are not used for permanent stains but mainly for wet mount.
EXAMINATION OF FEACAL SPECIMEN
Examination of stool specimen in the laboratory is usually in two phases. Macroscopic and microscopic, both of which are important, as each has special diagnostic features to reveal.
Consistency of the stool gives an indication to the type of organism likely to be present. Trophozoites (motile stages) of protozoa are often found in liquid or semi-formed stool. While the cysts are rare in the formed specimens.
Helminth eggs are common im _ formed stool specimens but are less in liquid specimen. Adult worms are often, beneath the specimens.
Blood or mucus patches, specific discolourations and any other non-uniform observation should be given specific special attention during examination. Presence of blood indicates bleeding in the gastro intestinal tract and occult blood may be suggestive of both parasitic infection or ulcer.
MICROSCOPIC EXAMINATION
A wet mount of the specimen is prepared and placed under the microscope for examination. Structures and
diagnostic features considered important include the following.
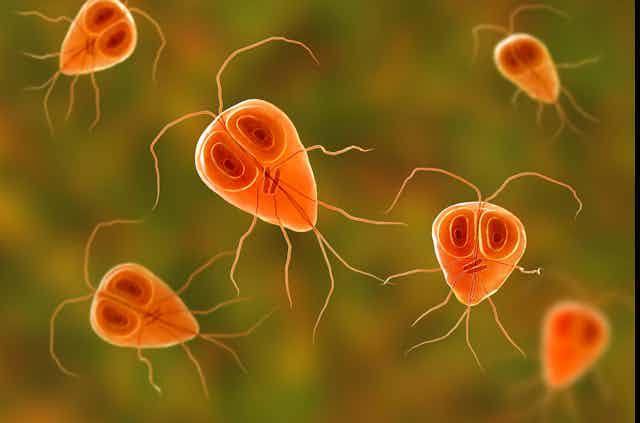
1. Trophozoite / cysts of protozoa
2. Helminth eggs/larvae
3. Blood cells,
i. Red Blood Cells – indicative of ulceration or hemorrhage
ii. White Blood Cells – Polymorphonucleay neutrophils (PMN) – Indicative of inflammation
iii. | WBC – eosinophills – indicative of immune response
iv. | Macrophages
4. Fungal cells – yeast cells
5. Plant cells – food particles
In examining the feacal specimen microscopically, two methods are often adopted – Direct smear and concentration method.
Direct smear technique is generally used for routine or diagnostic work in the laboratory. It is based on the premise that there is enough mixing in the stomach and intestinal tract before the stool is passed. A small portion of the stool specimen is usually placed on a clean glass slide with the applicators stick emulsified with physiological saline.
This is covered with coverslip and viewed under the microscope. Using x 10, then x 40 objective lens, and in most cases under low light intensity.
The feacal portion emulsified should not ‘ be too much to avoid thick preparation which makes parasite identification difficult, neither should it be too small.
This direct wet mount is to detect motile trophozoite stages of protozoa which are wholly pale and transparent hence the need for the low light intensity. Helminth eggs, larval stage protozoan cysts are equally observed in wet preparations, After checking the wet mount for trophozoites, iodine can be added to reduce or eliminate motility.
In some cases, fresh preparation can be made with lugol’s iodine or D’ Antoni’s Iodine which is better than Gram’s iodine. Nait’sbM buffered methylene blue can be used to stain the nuclear materials in cysts.
In concentration methods, there are two approaches – sedimentation and floatation. The two methods separate rotozoan and helminth eggs from feacal debris by the use of specific gravity. For floatation, the parasites are recovered in the surface film and the debris remain at the bottom.
This gives, clean preparation but some helminth large eggs, (Tapeworm eggs), operculated eggs (paragonimus eggs) and unfertilized Ascaris eggs are not concentrated in this form.
Floatation technique is not as often used as sedimentation method. Sedimentation technique is easier to perform as it depends on gravity or low specific gravity solution using formalin – ether or acid – ether as the solution.
DETECTING BLOOD PARASITES
Some parasites – microfilariae, and trypanosomes are detected in fresh blood but others like plasmodia require permanent stains. Specific identification also require permanent stains. In detecting blood parasites, two types of blood films are used each providing a different kind of information.
While thick films allow a large amount of blood to be examined increasing the possibility of detecting light infections, thin films are desired for malaria parasites with distinct morphological characteristics only observed inside each cell.
In blood examination, the use of clean greese free glass slides. Where blood is to be sent to the lab in uncoagulated forms, anti coapulants should be used and the most common is EDTA (Sequestrene).